The global healthcare landscape is undergoing a profound transformation as populations age and chronic disease prevalence rises. Remote patient monitoring (RPM) has emerged as a critical solution, enabling healthcare providers to track patient health metrics continuously without requiring frequent hospital visits. For elderly individuals and those managing long-term conditions, this technology represents a paradigm shift—transforming reactive emergency care into proactive, data-driven health management. With over 53 million caregivers in the United States alone supporting loved ones, and the UK’s population aged 80 and over exceeding 3.2 million, the demand for accessible, effective monitoring solutions has never been more urgent. RPM technologies bridge the gap between clinical expertise and daily living, offering patients independence while ensuring safety and timely intervention when health metrics indicate concern.
Remote patient monitoring systems: core technologies and IoT infrastructure
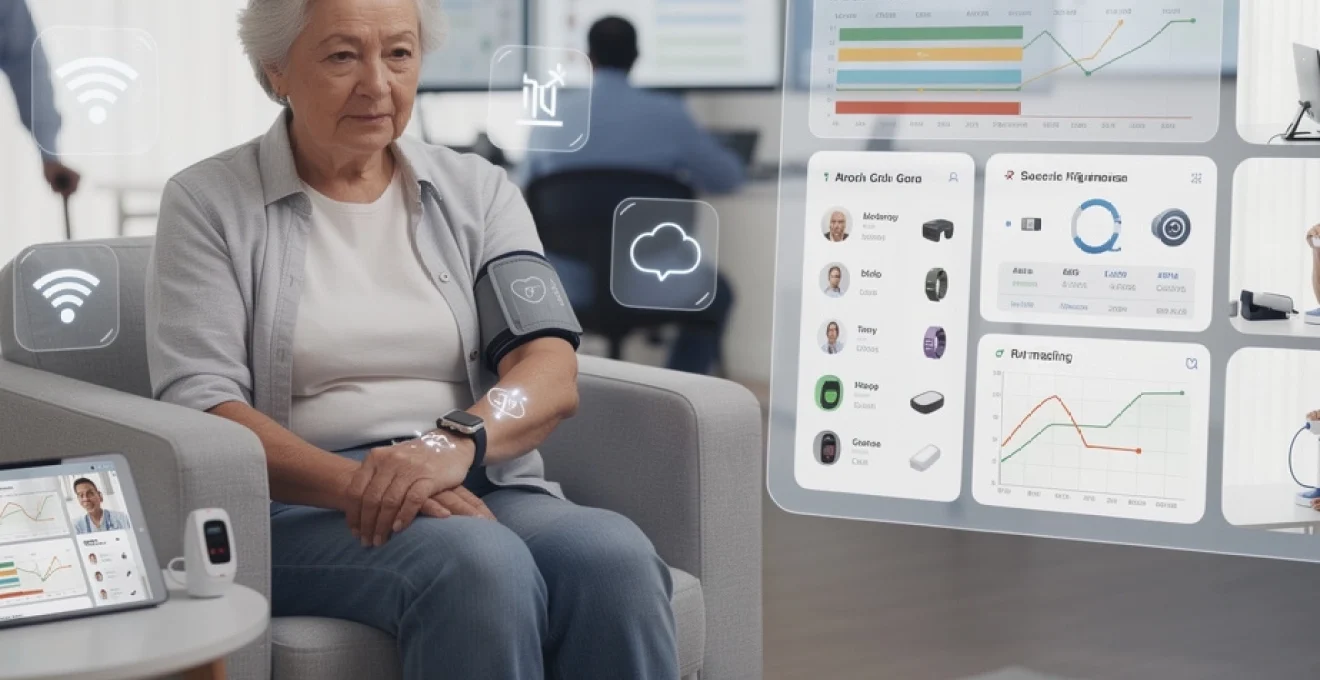
Remote patient monitoring relies on an interconnected ecosystem of devices, connectivity protocols, and data platforms working seamlessly together. At its foundation, RPM systems collect physiological data from patients in their homes or care facilities, transmit this information securely to healthcare providers, and enable clinical teams to review, analyse, and act upon the data. This infrastructure has become increasingly sophisticated, incorporating Internet of Things (IoT) principles that allow multiple devices to communicate within a unified health ecosystem. Understanding these core technologies helps explain how RPM delivers such transformative benefits for vulnerable patient populations.
Wearable biosensors and continuous vital sign tracking devices
Modern wearable biosensors represent a significant leap forward from traditional monitoring equipment. These devices continuously track vital signs including heart rate, respiratory rate, body temperature, and blood oxygen saturation without requiring active patient participation. Unlike conventional hospital monitors that tether patients to bedside equipment, wearable biosensors allow unrestricted movement while maintaining clinical-grade accuracy. Many incorporate accelerometers and gyroscopes to detect falls or changes in activity patterns, particularly valuable for elderly patients at risk of injury. The latest generation of biosensors can measure electrodermal activity, providing insights into stress levels and autonomic nervous system function—metrics that prove especially useful for patients recovering from cardiac events or managing anxiety disorders.
Cellular and Wi-Fi connectivity protocols for medical data transmission
The reliability of RPM systems depends fundamentally on robust connectivity infrastructure. Most contemporary devices employ either Wi-Fi networks or cellular protocols (4G LTE and increasingly 5G) to transmit health data to cloud platforms. Wi-Fi connectivity offers high bandwidth and low cost for patients with home internet access, while cellular connections provide crucial coverage for those in rural areas or without broadband infrastructure. Redundant connectivity options ensure that critical health alerts reach clinical teams even when one network experiences disruptions. Advanced systems automatically switch between connection types to maintain uninterrupted data flow. Some RPM platforms utilise Bluetooth Low Energy (BLE) technology for device-to-smartphone communication, with the smartphone then serving as a gateway to transmit aggregated data via cellular or Wi-Fi networks, optimising battery life on medical devices.
Cloud-based health data platforms and FHIR interoperability standards
Cloud infrastructure provides the scalable computing power necessary to process vast quantities of patient data in real time. These platforms employ sophisticated algorithms to identify concerning trends, trigger alerts when readings exceed predetermined thresholds, and present actionable information to clinicians through intuitive dashboards. Interoperability has historically challenged healthcare technology adoption, but the Fast Healthcare Interoperability Resources (FHIR) standard has emerged as a solution. FHIR enables different health IT systems to exchange data seamlessly, allowing RPM platforms to integrate with electronic health records, laboratory systems, and pharmacy networks. This standardisation ensures that remote monitoring data becomes part of a patient’s comprehensive medical record, accessible to all authorised providers across the care continuum.
Fda-cleared RPM devices: withings BPM connect and KardiaMobile ECG
Regulatory approval provides essential quality assurance for medical monitoring devices. The Withings BPM Connect represents a new generation of home blood pressure monitors—featuring cellular connectivity, automatic data transmission, and clinical validation for accuracy. Its one-button operation makes it accessible for elderly users with limited technical proficiency. Similarly, the KardiaMobile ECG device, validated by the US Food and Drug Administration, enables
single‑lead electrocardiogram recordings to be captured anywhere. Patients simply place their fingers on the sensor for 30 seconds, and the tracing is transmitted to a smartphone app and onwards to clinicians. This kind of remote ECG monitoring is particularly valuable for detecting intermittent arrhythmias such as atrial fibrillation, which may not appear during short, in-clinic tests. For older adults at high risk of stroke, having an FDA‑cleared device at home means suspicious palpitations can be documented and reviewed quickly, often leading to earlier diagnosis and treatment.
Chronic disease management through telehealth monitoring
For many elderly and sick patients, the greatest value of remote monitoring lies in long-term chronic disease management. Rather than relying on occasional clinic visits and subjective symptom reports, clinicians can see how conditions behave in day-to-day life. Continuous or high-frequency data capture enables earlier interventions, fewer emergency admissions, and more personalised treatment plans. In practice, this means remote patient monitoring becomes a cornerstone of care for diabetes, heart disease, respiratory illness, and hypertension.
Continuous glucose monitoring for type 2 diabetes patients using dexcom G6
Continuous glucose monitoring (CGM) has transformed how we support people living with type 2 diabetes, particularly older adults who may struggle with finger-prick testing. Systems like the Dexcom G6 measure glucose levels in the interstitial fluid every few minutes via a small sensor worn on the skin. Readings are transmitted to a smartphone or receiver and can be shared automatically with caregivers and clinicians. Instead of a handful of daily measurements, care teams see full 24‑hour glucose profiles, including overnight trends.
This rich stream of data helps providers optimise medication regimens, especially insulin, and identify patterns such as dawn phenomenon or post-meal spikes. For patients, real‑time alerts for high or low readings reduce fear of hypoglycaemia and support safer everyday living. Families can also receive notifications if glucose drops dangerously, providing peace of mind when an elderly loved one lives alone. Over time, CGM‑based remote monitoring has been associated with lower HbA1c levels and reduced hospitalisation rates—tangible proof that data-driven diabetes care works.
Cardiac arrhythmia detection with apple watch ECG and remote cardiologists
Cardiac rhythm problems are often sporadic, making them hard to capture during short appointments. Wearable devices such as the Apple Watch with ECG capability offer an elegant remote monitoring solution. When a patient experiences palpitations, dizziness, or shortness of breath, they can trigger a single‑lead ECG recording from their wrist. The resulting tracing is analysed on-device for signs of atrial fibrillation and stored in the Health app, where it can be exported securely to their cardiologist.
In more advanced telecardiology programmes, Apple Watch ECG data streams to cloud platforms where remote cardiologists review suspected arrhythmias. Automated algorithms flag concerning episodes, while clinicians interpret ambiguous cases. This blend of artificial intelligence and human expertise reduces unnecessary clinic visits while ensuring serious rhythm disturbances are not missed. For frail elderly patients who would otherwise face repeated trips to hospital, wrist-based ECG monitoring can be the difference between timely anticoagulation and a preventable stroke.
COPD exacerbation prevention via SpO2 monitoring and spirometry data
Chronic obstructive pulmonary disease (COPD) is a leading cause of hospital admissions among older adults, particularly during winter respiratory virus surges. Remote patient monitoring tackles this challenge by tracking key indicators of respiratory status at home. Pulse oximeters measure peripheral oxygen saturation (SpO2) and heart rate, while portable spirometers assess lung function parameters such as FEV1. Patients perform simple daily tests, and results upload automatically to clinical dashboards.
When algorithms spot a downward trend in SpO2 or spirometry, or a combination of increased respiratory rate and symptom scores, alerts prompt early intervention. Clinicians can adjust inhaler regimens, prescribe rescue steroids or antibiotics, and arrange same‑day reviews before an exacerbation escalates. Think of it as a “smoke alarm” for lung health: instead of discovering the fire once the house is engulfed, remote monitoring identifies the first wisps of smoke. This approach not only prevents hospitalisations but also preserves functional independence and quality of life for older adults living with COPD.
Hypertension control using automated blood pressure cuffs with bluetooth integration
Hypertension remains one of the most common and modifiable risk factors for stroke, heart attack, and kidney disease. Yet in traditional models, blood pressure control is often poor because treatment decisions rely on infrequent clinic readings that can be distorted by “white coat” effects. Automated home blood pressure cuffs with Bluetooth or cellular connectivity solve this problem by capturing multiple readings across different times and days. Devices like Withings BPM Connect or Omron smart cuffs sync seamlessly with smartphones and RPM platforms.
Clinicians can review weekly or monthly blood pressure summaries, spotting whether medications are truly effective in real-world conditions. For patients, easy-to-use devices and clear app interfaces encourage adherence to monitoring protocols. Remote titration programmes go a step further: pharmacists or nurses adjust dosages based on predefined protocols and remote readings, often achieving target blood pressures faster than traditional care. For elderly patients who may have limited mobility or live far from clinics, this kind of remote hypertension control can prevent serious cardiovascular events without adding travel burden.
Fall detection systems and emergency response automation for elderly care
Falls are one of the most feared events in later life, with around half of people over 80 experiencing at least one fall per year. A serious fall can trigger a cascade of complications—from fractures and hospital stays to long-term loss of independence. Remote monitoring technologies now play a central role in fall detection and emergency response, especially for older adults living alone or in care homes. Instead of relying solely on scheduled check-ins, sensors and intelligent systems can summon help the second something goes wrong.
Accelerometer-based fall sensors and medical alert systems like philips lifeline
Wearable fall detectors often use accelerometers and gyroscopes to distinguish between normal movement and a sudden impact followed by inactivity. When the device detects a likely fall, it automatically sends an alert to a monitoring centre, caregiver, or family member. Systems such as Philips Lifeline combine fall detection with a classic medical alert button, so the wearer can also call for help manually after a minor incident or if they feel unwell. Some models are water-resistant, allowing continuous use in high-risk areas such as bathrooms.
From the caregiver’s point of view, these devices provide reassurance that they will be notified even if a loved one cannot reach the phone. For the patient, knowing that help is just a button press—or even an automatic alert—away can restore confidence to move around the home. This matters because fear of falling can paradoxically increase risk by leading to inactivity, muscle loss, and poorer balance. By combining continuous monitoring with rapid response, accelerometer-based fall systems help maintain both safety and independence.
Ai-powered video analytics for gait analysis and balance assessment
Beyond reacting to falls, advanced remote monitoring aims to predict and prevent them. AI-powered video analytics can analyse how a person walks—assessing gait speed, symmetry, stride length, and balance. Using cameras placed discreetly in hallways or common areas of care homes, algorithms build a baseline of normal movement, then flag subtle changes that may indicate rising fall risk. For example, a shorter stride or increased sway when turning might prompt a physiotherapy review before a fall occurs.
These systems act like a continuously observing physiotherapist who never gets tired or distracted. Care teams receive periodic reports and targeted alerts rather than raw video streams, helping them focus on residents who most need intervention. Understandably, privacy is a major concern, so responsible implementations use privacy-preserving techniques such as skeletal tracking models instead of identifiable video. When done correctly, AI-based gait analysis allows providers to act early—adjusting medications that cause dizziness, suggesting mobility aids, or adapting the environment to reduce hazards.
Geofencing technology and GPS tracking for dementia wandering prevention
For people living with dementia, the risk of wandering and getting lost is a constant worry for families and care providers. Geofencing and GPS tracking technologies offer a humane way to support freedom of movement while reducing danger. Wearable GPS devices—often in the form of watches, pendants, or shoe inserts—communicate with smartphone apps or monitoring centres. Caregivers can define safe zones, such as the home, garden, or local neighbourhood. If the wearer crosses the virtual boundary, an automatic alert is triggered with their real-time location.
This geofencing approach balances autonomy and safety: instead of locking doors or restricting outings, you allow the person to move within agreed limits, stepping in only when necessary. For family caregivers who may live at a distance or juggle work responsibilities, knowing they will be notified if their loved one wanders too far brings immense peace of mind. In some programmes, emergency services have direct access to location data during missing person incidents, shortening search times and improving outcomes.
Clinical workflows and care coordination in RPM programmes
Remote monitoring technologies only deliver real value when they fit smoothly into clinical workflows. If data arrives in chaotic formats or without clear responsibility for follow-up, clinicians can quickly feel overwhelmed. Successful RPM programmes therefore combine devices, software platforms, and well-defined protocols for who does what, when, and based on which thresholds. This is where reimbursement models, dashboards, EHR integration, and new care models such as virtual wards come into play.
CPT codes 99453, 99454, and 99457: medicare reimbursement models
In the United States, Medicare reimbursement has been a major driver of RPM adoption, particularly for elderly patients with chronic conditions. Specific Current Procedural Terminology (CPT) codes support billing for different aspects of remote monitoring. CPT 99453 covers the initial set-up and patient education on use of devices. CPT 99454 reimburses for the supply of devices and the automated transmission of physiologic data over a 30‑day period. CPT 99457 (and its companion code 99458) support reimbursement for clinical staff time spent reviewing RPM data and communicating with patients each month.
These codes acknowledge that teaching a patient to use a blood pressure cuff correctly, reviewing their readings, and making treatment decisions are all legitimate clinical activities. For providers, understanding and correctly applying these RPM reimbursement models is essential to sustain programmes financially. For patients and caregivers, Medicare coverage removes a key barrier to access by reducing out-of-pocket costs. As other payers and international health systems develop similar frameworks, we can expect remote patient monitoring to become a standard part of chronic disease management.
Clinician dashboards and alert algorithms for abnormal vital sign thresholds
With potentially thousands of patients transmitting data every day, how do clinicians avoid drowning in information? The answer lies in well-designed dashboards and alert algorithms that prioritise what truly matters. RPM platforms aggregate readings into intuitive interfaces, often highlighting patients with out-of-range values, rapid changes, or missing data. Thresholds can be customised to each individual—for example, a slightly lower oxygen saturation might be normal for a COPD patient but alarming for someone else.
Alert algorithms work like a triage nurse, surfacing only those cases that need human review. Some systems use machine learning to differentiate between a one-off anomalous reading and a meaningful trend, reducing “alarm fatigue” for staff. Clinicians can drill down from population-level overviews to detailed timelines for a single patient, seeing how medications, activity, and symptoms intersect. When an issue is identified, secure messaging or telehealth visits allow rapid follow-up, often the same day. This combination of automation and human judgement is what turns raw RPM data into actionable care.
Integration with electronic health records: epic and cerner RPM modules
For remote monitoring to support truly coordinated care, data must flow into the same electronic health record (EHR) systems clinicians use every day. Major vendors like Epic and Cerner now offer dedicated RPM modules or integration toolkits. These enable remote readings—such as home blood pressure scores, weight data, or glucose trends—to appear alongside lab results, medication lists, and clinic notes. From a clinician’s point of view, this reduces the need to juggle multiple logins and systems.
Integration based on standards like FHIR also supports shared decision-making: during a telehealth or in-person visit, a doctor can show the patient their own trends within the EHR, reinforcing the link between lifestyle choices and health outcomes. Moreover, embedded RPM data can trigger clinical decision support alerts—such as reminders to adjust therapy if blood pressure remains uncontrolled after a set period. When EHR and remote monitoring platforms work in harmony, care teams can coordinate more effectively across primary care, specialists, and community services.
Virtual ward models and hospital-at-home programme protocols
Virtual wards and hospital-at-home programmes take remote patient monitoring a step further by shifting entire episodes of care out of the hospital. In these models, patients who would traditionally be admitted—such as those with heart failure exacerbations, pneumonia, or post-surgical needs—are instead monitored intensively at home. RPM devices capture vital signs multiple times per day, while nurses and doctors review dashboards, conduct video rounds, and visit in person when necessary.
Protocols define which patients are eligible, how often data is reviewed, and what escalation steps to follow if readings deteriorate. For example, a heart failure “virtual ward” might require daily weight, blood pressure, and symptom scores, with automatic alerts for rapid weight gain indicating fluid retention. Clinical teams often describe these programmes as “bringing the ward to the patient” rather than the other way around. Early studies have shown that well-run virtual wards can reduce length of stay, lower readmission rates, and improve patient satisfaction—particularly valuable for older adults who face higher risks of delirium and functional decline in hospital settings.
Data security compliance: HIPAA, GDPR, and patient privacy safeguards
Because remote patient monitoring depends on continuous data flows from the home, robust privacy and security safeguards are non-negotiable. In the US, RPM providers and healthcare organisations must comply with the Health Insurance Portability and Accountability Act (HIPAA), which sets strict rules for protecting personal health information. This includes encrypting data in transit and at rest, implementing access controls and audit logs, and having clear business associate agreements with technology vendors. In practice, that means only authorised clinicians can view patient dashboards, and every access is traceable.
In Europe and other regions influenced by it, the General Data Protection Regulation (GDPR) adds further requirements around consent, data minimisation, and the right to access or delete personal information. Patients should know exactly what is being monitored, who can see their data, and for what purposes it will be used. Transparent privacy notices and simple consent workflows help build trust, especially among elderly users who may worry about being “watched” all the time. From a technical perspective, best practice includes regular security testing, prompt patching of vulnerabilities, and strong identity verification for both patients and clinicians. When patients understand that remote health monitoring is designed to keep them safe—not to invade their privacy—they are far more likely to engage fully with RPM programmes.
Clinical evidence and patient outcomes from RPM implementation studies
Remote monitoring is no longer just a promising concept; a growing body of clinical evidence shows real benefits for elderly and chronically ill patients. Multiple randomised controlled trials and large observational studies have demonstrated reductions in hospital admissions, emergency department visits, and overall healthcare costs when RPM is implemented thoughtfully. For example, heart failure remote monitoring programmes using daily weight and symptom reporting have reported relative reductions in hospitalisations of 20–30% in some cohorts. Similarly, home blood pressure monitoring combined with telehealth titration has led to significant improvements in blood pressure control compared with usual care.
Diabetes studies using continuous glucose monitoring and remote coaching have shown lower HbA1c levels and fewer episodes of severe hypoglycaemia. Among COPD patients, remote SpO2 and symptom tracking have been associated with earlier treatment of exacerbations and shorter lengths of stay when admissions are needed. Importantly, many of these benefits extend beyond raw clinical metrics. Surveys consistently show that patients feel more supported and more in control of their conditions when enrolled in RPM programmes. Caregivers, too, report reduced anxiety knowing that a clinical team is watching over their loved one in the background.
Of course, not every implementation is equally successful. Studies also highlight the importance of user-friendly devices, adequate training, reliable connectivity, and clear escalation pathways. Programmes that simply ship devices to patients without strong clinical follow-up often fail to deliver meaningful results. The most effective remote monitoring initiatives are those that blend technology with human relationships: nurses who phone when readings change, doctors who adjust treatment promptly, and support teams who troubleshoot technical issues. When we combine evidence-based protocols with compassionate care, remote monitoring can help elderly and sick patients live safer, more independent lives while keeping healthcare systems sustainable.